Muranski Lab
Principal Investigator
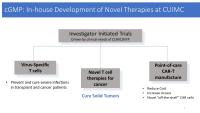
Recent advances in immune-oncology and cell-based immunotherapy have vividly demonstrated the enormous potential of the immune system to control and eradicate even otherwise refractory cancer. Our lab contains basic/translational research unit and the Columbia Cellular Immunotherapy Laboratory (CITL) capable of clinical-grade manufacturing and operating under current Good Manufacturing Practice (cGMP). We focus on basic science of tumor immunology and on creation of novel tumor- and virus specific T cells for use in patients with malignancy or refractory viral infections. The overarching goal of this work is to initiate and execute investigator-initiated early phase clinical trial of adoptive immunotherapy at CUMIC/NYP.
Our Research
The following research areas are explored in the Muranski Lab at Columbia University Irving Medical Center:
Basic Tumor Immunology
We focus on realistic murine models of adoptive immunotherapy for large solid tumors, thus mimicking clinical situation of patient with advanced cancer. We aim to understand how CD4+ T helper cells can contribute to anti-tumor responses. Using a novel TCR transgenic TRP1 model we have discovered that tumor-specific CD4+ T cells can eradicate even advanced rapidly growing murine melanoma tumors. This was particularly striking when CD4+ T cells were in vitro polarized into a Th17 subset. Paradoxically, this anti-tumor effect of Th17 cells was critically dependent on their ability to secrete interferon (IFN) γ in vivo, suggesting multi-potency and late plasticity. Tumor-specific Th17 cells, despite phenotypic features of terminal differentiation, were long-lived, highly active and displayed a core molecular signature reminiscent of early memory CD8+ T cells with stem cell-like properties. Thus, in vitro programming of CD4+ effectors is critical for the in vivo efficacy of those cells upon adoptive transfer.
Translational Tumor Immunology
Based on the animal model experience, we hypothesize that harnessing the power of tumor specific CD4+ T cells might be crucial for improved outcomes of adoptive immunotherapy in patients with cancer. Our research involves novel priming, programming, expansion, and isolation strategies for reliable induction of multi-epitope specific CD4+ T cells targeting several common tumor antigens expressed in solid and hematological malignancies. We use advanced humanized mouse models to test the activity of human T cells in vivo. This work will serve as a pre-clinical foundation for the upcoming clinical trials in patients with cancer and hematological malignancies.
T cell Adoptive Immunotherapy for Patients (cGMP)
Cellular Immunotherapy Laboratory (CITL) at the Columbia University Medical Center (CUMC)/Herbert Irving Comprehensive Cancer Center (HICC) was established in July of 2017 and serves as a foundation for the comprehensive cell therapy program at CUMC/HICC. CITL operates a fully staffed and functional manufacturing facility compliant with the cGMP regulations. The laboratory is capable of process development and production of immune effectors for patients enrolled in clinical studies at our institution.
In addition, CITL supports over twenty industry-sponsored clinical trials involving cell therapy products, including CAR- and TCR-engineered T cells, VST cells and cell-based vaccines.
Open Studies:
“Phase I Study of Adoptive Immunotherapy of Refractory Viral Infection With ex vivo Expanded Rapidly Generated Virus Specific T (R-MVST) Cells”. https://clinicaltrials.gov/ct2/show/NCT05183490(link is external and opens in a new window)
This is the first investigator-initiated trial utilizing anti-viral T cells generated in-house at Columbia. R-MVST cells target cytomegalovirus (CMV), Epstein-Barr virus (EBV), BK polyomavirus and adenovirus (Ad) in bone marrow transplant (BMT) and solid organ transplant recipients.
Pipeline (Under Development)
Polyomavirus-specific T cells for therapy of BK and JC-related disease
Dr. Muranski has previously developed polyoma-virus specific T (PyVST) cells targeting John Cunningham (JC) virus-related Progressive Multifocal Leukoencephalopathy (PML). Patients with PML in the context of hematological malignancy or rituximab use typically face a dismal prognosis with app. 80-90% mortality and a median survival of 3 month from diagnosis. The clinical trial of PyVSTs has recently completed accrual (NCT02694783) with excellent safety record and 7/12 response rate (Lancet Neurol . 2021 Aug;20(8):639-652. PMID: 34302788 PMCID: PMC8395368). Based on this experience, we are developing a new generation of PyVST cells with enhanced potency, targeting related BK and JC Polyomaviruses for use in solid organ transplant recipients and other immunocompromised patients.
TIL-like CD4+ T cell for adoptive immunotherapy of solid and hematological malignancies
Novel cytotoxic CD4+ T cells targeting common and mutated tumor antigens derived from autologous or allogeneic peripheral blood as a source.
Lab Members
Rodica Ciubotariu, MD, PhD
- Director of Clinical Operations; cGMP
Mithil Soni, PhD
- Associate Research Scientist
Prabesh Khatiwada, PhD
- Postdoctoral Fellow
Hei T. Chan, RN
- Research Nurse, Immune Effector and Cell Therapy Program Lead
Agata Jurewicz, MS
- Quality Assurance Specialist, CITL cGMP
Jian B. Pan
- Senior Technician, CITL cGMP
Emma Senner
- Technician B, CITL cGMP
